The terminology of tubular breasts is synonymous with tuberous breasts. This condition exists from birth presents at puberty and becomes more visible with breast growth. Although the breasts are functionally normal, however, they are cosmetically different. It may present in more than one member of a family. Some tribes in Africa with a large number of intermarriages have a prevalence of tubular breasts, which can reflect a genetic predisposition. The tubular breasts are seen as cosmetically desirable and attractive in some cultures.
The patients’ presentation to my clinic includes statements like; my breasts look pointy, and I do not like my breasts’ shape, size, and asymmetry. In others, they inform me that they do not feel that their breasts are feminine enough. In some patients they also add; I do not feel comfortable changing in common rooms in the gym or the swimming pool.
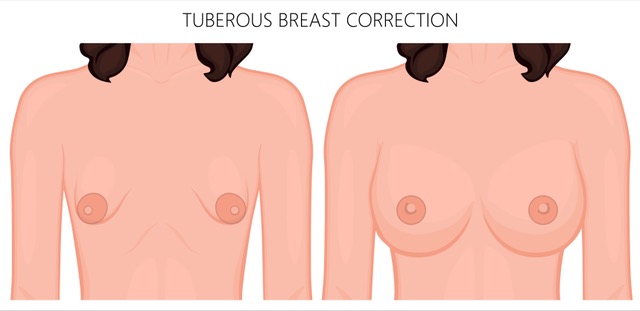
When examining patients with tubular breasts, the breasts may be narrow, pointy, and not unusually small relative to the patient stature and height. Asymmetry is common and the cleavage is wide, the areola is disproportionately large and protrudes, whilst in some cases constriction in the lower aspect of the breast causes the nipples to point down. In my opinion, this causes constrictional Ptosis of the nipple as a result of lack of tissue rather than tissue excess or laxity as in the usual ptotic (droopy) breast. In the more severe cases the breast/s may be almost absent this is termed grade IV.
In the more very mild forms of tubular breasts, grade I, the patient may notice cyclical variation, which mirrors their menstrual cycle. The tuberosity appears less obvious in the last few days of the menstrual cycle, i.e. nearer to day 25-28 in a 28-day cycle as the breasts are fuller partly due to fluid retention.
The treatment of tubular breasts is often surgical. The psychological impact must taken into consideration as much as the cosmetic effects of the condition as an indicator for surgery. The treatment can be in one or two stages. The choice of procedure is patient age dependent and is influenced by the severity of the presentation and most importantly, the patient’s choice. In addition, the surgeon’s experience has a bearing on the procedure choice.
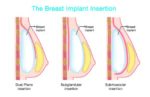
One-stage procedures are likely to involve in the majority of cases shaped breast implants (teardrop); however in a very selected small number of cases where there is less constriction of the lower pole of the breast, round implants may also be feasible. In the last 18 years, I have used both shapes of implants, and patients have been very happy with the outcome. Adjunctive procedures including internal breast tissue scoring to improve the protuberant areolas.
Fat transfer (Lipo-filling, Lipo-modelling) may also be of benefit and must be taken into consideration as a sole treatment, however, it will warrant more than one episode. In addition, mastopexy (breasts uplift), plays a significant role in a large number of patients with tubular breasts.
The two-stage technique may be of more benefit in the younger patient when the breast growth has not concluded or when significant asymmetry exists. The completion of breast growth may vary between ages 21-23.
The 2 stages of surgery will include a first stage of tissue expansion using expandable silicone prostheses, which will contribute to the widening of the narrow base of the breast and add more fullness and volume until the breast growth is nearer its final stage. The expanders will be inflated over a period of time, which is individually tailored. The inflation is performed through a port that is buried under the skin. This port is part of the expander and is placed intra-operatively over the side of the rib cage in the first stage.
Not all patients will need a second stage. However, in those patients needing a second stage, this may involve the expander prosthesis removal and replacement with silicone implants; a mastopexy (breasts uplift), is performed in that patient whose breasts need to undergo this surgery. However the expander implants may be retained and the mastopexy is performed with the device in situ, and the expansion ports removed. Nonetheless, if a second stage is not warranted the expander ports could be removed through a separate cut under local anaesthetic. Fat transfer is of great value in adding refinement to the outcomes of the surgery.
In my 21 years as a consultant dealing with tubular breasts patients I find that the teenage patients whom I have treated since their early years have blossomed into young successful confident adults. This is a moral reward that cannot be quantified and can only be termed as priceless.
What to expect:
The surgery is carried out at an accredited hospital under a general anaesthetic; the hospital stay is 1 night. The dressings are removed and the dissolvable stitches are trimmed short after 10-12 days. The anticipated recovery in most patients is in the majority of 3 weeks.
In the patients who have undergone expander insertions, inflation is usually carried out at the second week and is tailored to each individual according to their breast needs and their availability. Once the inflation is finished the second stage when required will vary on the patient’s age and the breasts tissue softening in preparation to the next stage.
Pain requirements vary between individuals; however, most patients find the pain limited and can be well controlled with appropriate painkiller tablets over the first few days after surgery.